First used in the 1940s antibiotics are one of the key advances in medicine. But their overuse has resulted in the development of resistant bacteria that no more respond to antibiotics. In fact, so tough has their resistance become over the last few years that some bacteria have become resistant even to the last-resort antibiotic called colistin. Why so? Because although the viruses and bacteria cause diseases with similar symptoms, they differ in the way they multiply and spread illness. Unlike viruses the bacterium is a living organism and acts like humans. When attacked it rebounds with greater vigour. Bacteria retaliate viciously by producing prodigiously - maybe as numerously as doubling their numbers in ten minutes. Small in size, simply designed and with diverse capabilities for survival - there are also some good, useful bacteria - they inhibit and flourish in almost any environment. According to a specialist in the field, "the use of broad-spectrum antibiotics or their long-term use, the hostile as well as friendly bugs are blasted and replaced with opportunistic bacteria or funguses which become troublesome colonisers inside the host." That bacteria are the most effective antidote to a number of illnesses is a misconception, which of late has come under sharper focus, given advanced research into how over-prescription of antibiotics has led to the growth of multi-drug resistant tuberculosis in countries like Pakistan, where, it's the myth among doctors and patients that all illnesses can be cured with antibiotics. The problem of resistant bacteria has been compounded by a host of negative factors, including wrong diagnosis by doctors, medical practice by charlatans said to number over 600,000 in Pakistan, false advertisements of antibiotics by profiteers, self-medication and their availability across the counter without a doctor's prescription.
Rightly then, the Medical Microbiology and Infectious Disease Society of Pakistan has advised that the issue be understood in all its positive and negative aspects at the public health level and by physicians. And the patients too should realise that the antibiotics are not the panacea for all fevers, and must desist from self-medication, or expect a prescription from their caregivers. Given certain symptoms it is no big problem to diagnose the disease and prescribe the remedy. But more often than not that is not being done. For instance, if the symptoms are cold, cough, body ache and fever, it is a case of viral infection, for which antibiotics are not required and home remedies would be effective enough. Likewise, sore throat, ear pain and mild fever or fever-cum-joints pain are also viral illnesses and don't need antibiotics. That said, one may concede there may be symptoms that confuse diagnosis, but it is the responsibility of a doctor not to prescribe an antibiotic unless there is clear evidence of a bacterial infection. According to specialists, a sore throat is viral in 80 percent of cases and bacterial only in 20 percent. Viral infections particularly of the upper respiratory system, say experts, "are usually self-limiting; they go away on their own after a few days or weeks and antibiotics have no role in their cure." If the government is doing enough to generate awareness about this problem, there is not much in evidence - a dilemma that tends to multiply as health is no more a federal subject and therefore deprived of the capacity to be taken up at federal level. Maybe the private sector, with the help of the mass media, can make up for this shortcoming by creating awareness on the misuse of antibiotics and the need for rapid diagnostics and legislation to prevent over-the-counter prescriptions.
BR100
15,103
Increased By
140.9 (0.94%)
BR30
42,619
Increased By
540.8 (1.29%)
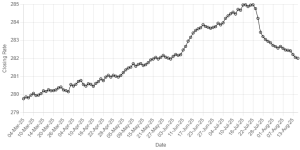
KSE100
148,196
Increased By
1704.8 (1.16%)
KSE30
45,271
Increased By
438.2 (0.98%)





















Comments
Comments are closed.